Seized with anxiety after days of painful cramps and bloody stool, Franco answered a call from the research company that had been dosing him with an experimental medication in exchange for money.
A staffer told him their tests showed one of his organs was inflamed and that a doctor needed to examine him.
“Is this something, like, permanent?” Franco asked.
“I’m not a doctor,” said the staffer. “I can give you the basic information of what I know… Because of the results that we got, you can’t continue on the trial, OK?”
“I mean, I don’t have an option, right?” Franco replied.
Like many professional clinical trial participants, Franco normally stays quiet about the side effects he experiences. He only gets paid in full if he completes the entire study. Leaving early because of an adverse reaction means he’ll forfeit more than $15,000.
Private companies in Canada are recruiting thousands of often economically desperate test subjects each year, using incentives that some experts say are both exploitative and push participants to lie. When that happens, data that Health Canada uses to approve drugs for the marketplace can be compromised.
Franco and his peers are part of an underground society of so-called “professional guinea pigs” lured by cash, referral bonuses, loyalty points, and other perks advertised by private companies to encourage them to sell their bodies for pharmaceutical research.
Canada is a hub for clinical trials
Canada is home to four per cent of the world’s clinical trials, and leads the G7 — a group of nations with advanced economies including France, the U.K. and the U.S. — in the number of trials per capita, according to the Canadian government.
Yet, unlike in some European countries, the government does not require national monitoring of participant enrolment. Participants can exploit that missing oversight, endangering their own health and tainting study data.
The government’s inspections of the trials themselves are limited. While Health Canada approves more than 1,000 trials every year, only a small fraction is inspected.
In a statement, Health Canada said it rigorously oversees clinical trials and works to protect the health and safety of participants.
The health agency said it aims to publish new regulations in spring 2025 that will “align with international best practices regarding trial oversight,” including changes that “would result in direct regulatory oversight of third parties involved in conducting clinical trials.” Health Canada did not say what those regulatory changes would be.
Meanwhile, the current lack of robust oversight has fostered a subculture of professional clinical trial participants who engage in deception to get paid.
Some cash-strapped participants lie about their health conditions in order to get selected, provide false urine samples at drug screenings and conceal side effects of the experimental drugs.

“A lot of people need the money,” says Franco, whose real name is being withheld at his request for fear of being blacklisted by drug testing firms from which he earns his living. “They have no problem lying.”
Carl Elliott, a bioethicist at the University of Minnesota who has long studied the ethics of clinical trials, calls it a “thoroughly exploitative system” that takes advantage of people living on the fringe.
“Why would someone blame Franco for the position he’s in?” he asks. “This is like blaming sweatshop workers for the poor safety conditions in sweatshops.”
‘Aggressive commercialization of research participation’
Three young women smile and embrace in a picturesque courtyard — perhaps on vacation — as beams of sunshine radiate behind them.
This is an ad by a contract research organization (CRO), a private firm paid by pharmaceutical companies to conduct clinical studies and manage the research process of their drugs.
“Experience a summer as hot as your bank account!” reads the ad. “With compensations reaching heights of up to $17,150, imagine the endless possibilities for making this summer one to remember!”
That shiny sum is meant to recruit post-menopausal and surgically sterile women to test a drug for the “treatment of overweight and obesity.”
The ad reflects the “blatant, aggressive commercialization of research participation,” says Trudo Lemmens, a professor of health law and policy at the University of Toronto who has studied ethics in clinical trial research.
To recruit participants in clinical trials, CROs advertise their studies in online classifieds, campus bulletin boards and public transit.
A CRO might offer participants more than $20,000 for completion of a trial, plus perks.

Clinical trials used to primarily be hosted by academic health-care institutions. But most are now carried out privately, including by CROs. Health Canada said it does not “readily” have the number of CROs that are operating in Canada.
They often conduct phase-one studies, where drugs are tested on healthy individuals to assess their safety. Sometimes, it is the first time humans have ingested the drugs.
Successful phase-one testing typically leads to subsequent trial phases before pharmaceutical companies submit the data to Health Canada for authorization to sell the medications.
It’s part hospital, part hotel, part prison, study subjects say
Participants may spend days or even weeks confined to the clinical trial site, where they undergo round-the-clock medical supervision and testing. They typically must follow a strict diet and sleep schedule, sometimes wearing matching clothes that display their participant numbers, which researchers call them by.
The IJB/Star interviewed more than a dozen current and former clinical trial participants as part of this investigation. Study subjects described trial sites as part prison, part hotel, part hospital. They see familiar faces from one trial to the next, exchange advice through networks of “study buddies” and online forums, and travel together across provincial lines to distant trial sites.
The companies use incentives to attract participants like Franco.
Syneos Health, which conducts clinical trials in Quebec, has offered prospective participants the chance to win an iPad upon registering for a study of their choice.
In a statement, Syneos Health said it has “a long-standing commitment to conducting safe and ethical trials, and participant welfare, safety, and data integrity remain our top priorities.”
“All clinical trials operate in a highly regulated, industry-wide ecosystem, with multiple layers of external oversight,” the statement said. “Independent research ethics boards mandatorily review and approve participant recruitment and compensation.”
Altasciences, which runs a clinical trial site in Montreal, has offered a points-based loyalty program featuring perks such as exclusive access to certain trials upon earning 10,000 or more loyalty points. The program is currently on hold, however, Altasciences’ website says.
‘Designed to lure poor people into the studies’
CROs offer study subjects “referral bonuses” of hundreds of dollars if they enlist their friends to participate in studies.
Altasciences and Syneos Health both offer test subjects their pay via reloadable, company-provided debit cards, according to their websites. Both companies say that one of the benefits of the debit card is that it does not require a personal bank account.
That appears “particularly designed to lure poor people into the studies,” says the University of Minnesota’s Elliott. “That seems obviously aimed at people who, for whatever reason, can’t get a bank account or don’t want a bank account,” such as participants who are in trouble with the law or immigration authorities.

Such perks can amount to a kind of psychological manipulation of participants and undermine their free and informed consent, says Kerry Bowman, a bioethicist at the University of Toronto who has served on a hospital research ethics board.
“The financial need of the participants is sufficiently high that it’s really compromising [their] autonomy,” Bowman says.
A 2018 U.S. study found more than one third of 178 research volunteers surveyed described trials as “a critical means of staying afloat,” with some relying solely on that income and “seeing no other alternatives to make ends meet.”
“I came from a very poor background,” says Julia Pak, a Toronto woman who describes her mother being homeless a couple of times when Pak was a kid and living in foster care for a stint as a teenager. She says doing studies was a way to make money, and she does not fault CROs or the clinical trial industry. “I’m completely capable of making my own decisions.”
Since moving from Mexico about two decades ago, Franco estimates he’s participated in more than 40 studies of pharmaceuticals ranging from opiates to psychiatric drugs for psychosis to a treatment for erectile dysfunction.
“They’re breaking the rules because they need a source of income, and they have identified clinical trials as the best way for them to have that“
In a good year, he earns more than $30,000 from studies and works odd jobs between trials, he says.
“If I see a good study, I cancel everything,” he says. “I make a lot more money doing studies than any other crappy job I had in Canada.”
Troubling lengths to get into studies
Franco and others will go to troubling lengths to get accepted into a trial.
Pak would stop taking her personal medication to get into trials.
“I don’t take my medications when I’m in the study, and then I let them give me whatever medications they need,” she said.
Franco stopped taking his regular drugs to get into studies, too. He has told study administrators he has no health conditions when in reality he has been diagnosed with serious psychological conditions. He says he has lied on questionnaires meant to gauge suicidality.
He has hidden or embellished his long history of recreational substance use to suit the needs of a study protocol. He says he even allowed “study buddies” to use his urine to pass drug screenings.

He and others interviewed for this story say they have downplayed the severity of side effects from trial drugs, or have not reported them at all, for fear of getting disqualified from studies.
Franco also says he uses diarrhea-inducing tea and has smoked meth to meet trial weight requirements. “I stopped using it because I was going crazy.”
Study participants, including Franco, have enrolled in back-to-back trials in violation of the typically 30-day “washout” periods between studies that allow a trial drug to clear a subject’s system before another trial begins. The rule is supposed to help ensure the integrity of the scientific data upon which drug approvals are based and protect participants from potentially dangerous drug interactions.
“They ask you, ‘have you done any studies in the last 30 days,’” says Franco. “Everybody says ‘no.’”
For years, Ontario trial subjects have routinely travelled back and forth between the GTA and Quebec to violate washout periods undetected. CROs had not traditionally shared information on participant enrolment across the provincial border, though that has begun to change lately.
Jill Fisher, a professor at the University of North Carolina at Chapel Hill’s Center for Bioethics who has interviewed hundreds of trial participants and staff, says they aren’t trying to sabotage science.
“They’re breaking the rules because they need a source of income, and they have identified clinical trials as the best way for them to have that.”
Possible models for better clinical trial oversight
Some countries in Europe require researchers to use registries to prevent clinical trial volunteers from over-enrolling in studies.
In France, a government participant registry established under law caps compensation for participants at about $9,000 (all figures CDN) per year.
In one trial alone, Franco says he earned $17,000.
“People are breaking the rules for a reason,” Fisher says. “There is this obsession with … looking at the participant, and looking at their activities, rather than seeing the structure.”
The U.K.’s Health Research Authority, meanwhile, requires the researchers of phase-one clinical trials to use The Over-Volunteering Prevention System (TOPS), a national database of participants verified through a National Insurance number or foreign passport number.
Today, TOPS operates for roughly just $16,000 annually.
There is no national registry in Canada. Oversight is left to the CROs.
To prevent breaches of washout periods, some CROs in Canada track the trial history of participants via fingerprint scans provided by a private service called clinicalRSVP. But some CROs choose not to use the service.
“The less holes you can have in that net, the more viable it can become,” says Darran Boyer, clinicalRSVP’s president and co-founder. “I think we’ve reached a mass where it’s definitely viable.”
Altasciences started using clinicalRSVP in May, joining CROs in the GTA and Syneos Health in Quebec.
Altasciences did not respond to numerous requests for an interview.
It is the government that should create a national verification network, says clinical researcher Dr. Thomas Shiovitz, who is also the president of a U.S.-based verification firm specializing in psychiatric and neurological clinical trials.
“Rather than have private companies like ours contain the information that can detect duplicate or professional subjects, it would be ideal for a governmental entity to require the registry of all phase-one subjects to protect their safety and the integrity of studies,” he says.
Health Canada said it “does not oversee the enrolment of participants in clinical trials.”
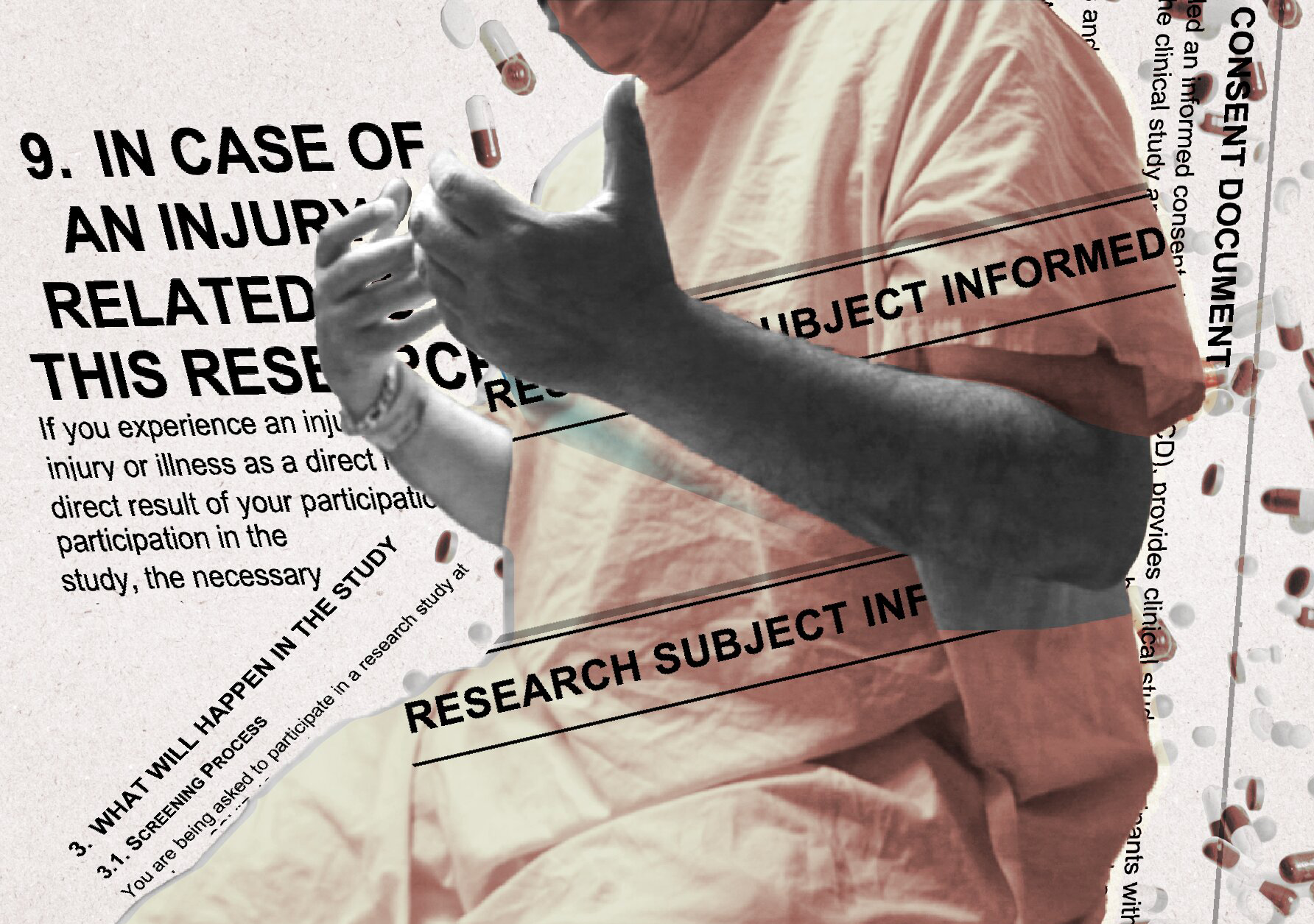
Each trial must be approved by a research ethics board (REB), an independent committee that ensures the “clinical trials are designed and conducted in an ethical manner, and that the rights of study participants are protected,” Health Canada said. Informed consent documents, as well as decisions about remuneration and incentives for participants, “fall under the purview of REBs.”
Clinical trials in Canada must involve qualified experts, “typically medical professionals,” to monitor participants.
But the University of Minnesota’s Elliott says that for there to be real oversight, “you need people actually inspecting the trial sites.”
Health Canada authorizes more than 1,000 trials each year
Health Canada said it uses a “risk-based approach” in selecting which trial sites to inspect, replacing its previous goal of inspecting two per cent of trials. “This allows Health Canada to focus its compliance and enforcement efforts on areas of the highest risk.”
Health Canada’s Clinical Trial Compliance Program (CTCP) employs a staff of just 11 inspectors. In 2022/23, the program inspected 55 clinical trials. Last fiscal year, they inspected 65.
Meanwhile, the health agency authorizes about 1,100 trials each year. Health Canada could not provide the number of active trials in Canada.
Among 460 trial inspections from 2012/2013 to 2020/2021, violations of research and ethics protocols were common, with 3,661 infractions. These trials are not limited to phase one studies and include those sponsored by hospitals and universities.
There were at least 33 trials with errors relating to the reporting or documentation of adverse drug reactions, including at least four failures to report “serious unexpected adverse drug reactions” to Health Canada within 15 days as required. There were at least 82 trials where there were issues with the informed consent process or records. In at least 109 trials, “not all individuals conducting the clinical trial had the education, training and experience to perform their respective tasks.”
Participants typically get paid in proportion to how much of a study they complete. They can get bonuses of up to thousands of dollars for finishing the entire study.
This completion bonus is “an incentive to hide [side effects], to do something against your better judgment,” says Lemmens, the U of T professor of health law and policy.
Lemmens said study participants “should be paid the full amount if they have to withdraw because of a serious side effect.”
Health Canada said clinical trials “incorporate various safety measures” and that, in addition to participant self-reporting of adverse events, there are also objective, physiological ways to detect adverse reactions.
“Prior to authorization of a drug, the totality of all nonclinical and clinical data from all clinical phases are assessed and considered,” Health Canada said.
For test subjects, a reluctance to stop
After being removed from the trial following his abdominal pain and nausea, Franco waited for around eight hours in an emergency room.
Sitting on the hospital bed, he described radiating pain as his doctor pressed on his abdomen.

That study — with the biggest payout of any he had ever been in — was supposed to be his last one before he retired for good. In his mid-fifties, Franco is drifting out of the common study age range of 18 to 55.
“I was supposed to use that money to live happily ever after.”
But with his reliance on the income — and few other options — he has been reluctant to stop.
After conducting testing, the doctor confirmed the study drug appeared to have caused his symptoms. But he should recover without permanent damage.
“Do you have any questions?” the doctor asked.
“No, no, no. I’m glad that I’m ready for the next one, ha!” Franco exclaimed.
Four weeks later, Franco enrolled in a new trial testing an allergy drug.
Behind the Reporting – Pulling the curtain back on Canada’s private clinical trial industry took more than two years of reporting, writing, data analysis and fact-checking. Collectively, reporters Max Binks-Collier, Masih Khalatbari, Charlie Buckley and Rob Cribb examined more than 50 ads from clinical research organizations and interviewed 14 clinical trial participants who we mostly found via Facebook and Google Reviews.
They reviewed videos, photos, dozens of consent forms, and other documents participants shared from their trials. Additionally, they analyzed clinical trial inspection data from Health Canada and the FDA and examined academic studies and publications from researchers who have been flagging concerns for decades.
This Story was originally published in the Toronto Star.

Bodies for Rent, a documentary directed by Habiba Nosheen in collaboration with the IJB, is out now!
Bodies for Rent takes us inside the hidden world of pharmaceutical drug testing. Directed by Habiba Nosheen in collaboration with the IJB, it’s available now on CBC Gem and Youtube via CBC Docs.

The Big Story podcast | “Professional guinea pigs”: Inside the world of clinical drug trials
The IJB’s Rob Cribb visits The Big Story on the Frequency Podcast Network to discuss our investigation into the clinical trials industry.
The Investigative Journalism Bureau is an impact-driven, collaborative newsroom that brings together professional and student journalists, academics, graduate students and media organizations to tell deeply-reported stories in the public interest.
Your support is crucial to our mission. By donating, you help us continue to uncover the stories that drive meaningful change and hold power to account. Join us in our commitment to high-quality, independent journalism.
- Feds vow to probe findings of IJB/Star/TVO investigation on mental health care for Indigenous people - 4 November 2024
- ‘Deeply troubling’: Ontario chiefs call for reforms to federal health program after Star/IJB investigation - 3 November 2024
- ‘I am deeply troubled’: Head of Ontario law society speaks out after Star/IJB investigation into sexual harassment among lawyers - 25 October 2024
- Inside Canada’s ‘exploitative’ clinical trial industry, where study participants say they’re incentivized to lie — even about medications’ side effects - 7 October 2024
- The hidden hate on campus: We tracked incidents at colleges and universities and found a growing problem - 10 March 2023
- She was suicidal, struggling with PTSD and addicted to alcohol. The help she needed was all under one roof - 9 December 2022